
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.

Heel pain is often associated with the condition known as plantar fasciitis. This common form of heel pain is the result of damage to, and inflammation of, the plantar fascia. The plantar fascia is the connective tissue on the sole of the foot that inserts at the heel bone, then spreads up to support the arch, and fans out to connect with each toe. Damage to the plantar fascia may be caused by wear from old age, obesity, shoes with inadequate support, and increasing physical activity too rapidly. Among the other causes are training on hard surfaces, standing for prolonged periods of time, and having flat feet or high arches. Plantar fasciitis typically causes pain in the inner/center part of the heel that worsens after periods of rest. Your podiatrist can offer various treatments to repair the plantar fascia, while reducing inflammation and pain. It is suggested that you contact one to seek treatment, as this condition may become chronic if the tissue does not heal properly.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Alan J. Spector from Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Being a parent involves caring for your child in every way you can. You make sure they are eating the right food, being nice to others, and staying out of any trouble. However, it is also important that you are watchful of their health, more specifically their foot health. Maintaining good foot health in childhood is important in preventing later conditions in life from happening. As children continue to develop, their feet require different techniques of care. Here are some various ways in which you can help your child’s feet stay healthy.
A baby needs a lot of care and attention overall, but the importance of their feet should never be forgotten. Before a baby turns one, their feet change and develop greatly. It is important that during this time, a mother avoids putting tight socks on their child. She should also encourage movement of their feet so the baby can begin to feel more comfortable using them.
As a baby enters the toddler years of his or her life, they are begin to walk around. When your baby begins to take those first steps, it is crucial that they are wearing protective shoes on their feet. As a mother that is observant of your child’s feet, you may notice changes in them. This is completely normal as the feet are becoming susceptible to the activity of walking. It is normal for a toddler to be a bit unsteady or to “walk funny” at first.
When your child grows out of their toddler years, it is important that you begin to show him or her how to care for their feet on their own. Practice with your child proper hygiene in order to prevent foot fungus or infection. Since children are constantly on the move, it is crucial to be cautious of any accidents or injuries that might occur. If an injury occurs, it is advised that you take your child to be examined by a doctor immediately. Since your child is still growing, particular injuries can shift the way in which a bone or other important part of the foot is developing.
Babies and kids are always changing and growing. Your job as a parent is to make sure they stay healthy and making sure they are properly maintained. This involves proper foot care and making sure the feet stay healthy. Following this guide, your child can live a long and happy life.

As a parent or guardian, you may wonder if your young child’s stance or gait is normal as they learn how to stand and walk. As your child grows, most issues will work themselves out, but there are some things you should monitor. When babies are born, they do not have arches, which is known as having flat feet. Typically, by the time a child is 6 years old, their arch is developed and visible when they stand. Around the age of 4, many children will have a small gap between their ankles when standing with their knees together (knock knees) which should go away by the age of 6 or 7 when their legs straighten out fully. If the gap is between both their knees and ankles, this is known as bow legs. This condition is commonly present in children less than 18 months old. Some young children walk on their tiptoes (tiptoe walking) until approximately 3 years of age, and thereafter will usually adopt the normal heel-to-toe walking pattern. Feet that turn in (in-toeing) or turn out (out-toeing) will usually start pointing straight by themselves when the child is roughly 8 years old. Regular check-ups with a podiatrist will help ensure that your child’s feet are developing normally. Also, if the issues mentioned here do not go away on their own, or you have any concerns about your child’s foot or ankle health, have your child examined by a podiatrist right away.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
If you have any questions, please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
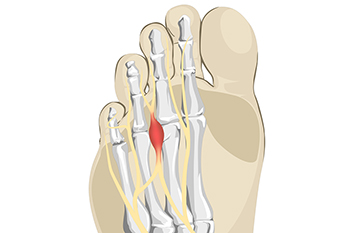
The pain from a foot condition that is known as Morton’s neuroma is generally found in the ball of the foot. A neuroma is another name for a pinched nerve or nerve tumor. It is often benign, and can grow and spread to other nerves in the foot. It is an ailment that affects the nerves between the third and fourth toes, and can cause severe pain and discomfort. Many patients describe the pain as feeling like a pebble or marble under the foot, and possibly cause difficulty in completing daily activities. Common reasons for this condition to develop can include frequently wearing high heels, and participating in running and jumping activities that can compress the feet in shoes. Additionally, medical conditions consisting of bunions and hammertoes may lead to getting Morton’s neuroma. A proper diagnosis consists of having a CT scan taken, or possibly an MRI. Many people have found mild relief when specific foot stretches are performed, and it can be beneficial to wear shoes that fit correctly. These types of shoes will have adequate room for the toes to move freely in, and this can help to achieve full range of motion and flexibility. Morton’s neuroma can be painful, and can hinder the ability to complete daily tasks. If you have pain in this part of your foot, it is suggested you consult with a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.

Getting a toenail infection can be easy, mainly because the fungus that causes it is very contagious. Spotting it is also easy. Infected toenails may change color to white, yellow, brown or green. They may become thickened, raise up off the toe, or crumble. Luckily, a number of simple precautions can help to keep fungal infections at bay. First, protect your feet by wearing shower slippers at pools, public showers, spas or gym locker rooms, all of which are common breeding grounds for fungi. If you have recently had a fungal infection, don’t wear shoes or slippers you wore during that time. Change your socks when they get sweaty. Keep your feet clean and dry, and wear canvas or mesh shoes that allow your feet to breathe. Give your shoes at least 24 hours to dry out before wearing them again. Avoid sharing personal items, such as nail clippers, shoes or towels, that may have picked up a fungus. Keep your feet moisturized, as fungi can enter through cracks or sores in the skin. Finally, be vigilant and check your toenails at least once a month for symptoms. If you need help in dealing with toenail infections, please consult a podiatrist.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Dr. Alan J. Spector of Shore Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Point Pleasant, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.